Understanding and Overcoming Vocal Cord Dysfunction
Most patients who come to my practice with Vocal Cord Dysfunction have never heard of it prior to their diagnosis. What is VCD? How did I get it? What are my treatment options? VCD is a disorder of the upper airway where the vocal cords fail to function properly, leading to difficulty breathing.
It is a surprisingly common condition that can cause immense physical and emotional distress to those who have it. Unfortunately, VCD can be difficult to diagnose, leaving many people feeling frustrated and confused about what is going on within their bodies. By understanding more about this condition and taking steps to seek help, you can find relief.
In this article, we’ll explore what vocal cord dysfunction is, the impact it can have on someone’s life, and ways to manage the symptoms. We’ll also look at how to identify the signs of VCD in you or someone you love and how to get the support you need to gain control of your breathing. Keep reading for everything you need to know about vocal cord dysfunction!
1. What Is Vocal Cord Dysfunction?
Vocal Cord Dysfunction (VCD) is an umbrella term for dysfunctional movement of the vocal cords. It goes by many names such as Paradoxical Vocal Fold Motion (PVFM), Exercise Induced Laryngeal Obstruction (EILO), Episodic Laryngospasm, Inducible Laryngeal Obstruction (ILO), and more. All of these terms are used to describe an intermittent, abnormal narrowing of the larynx.
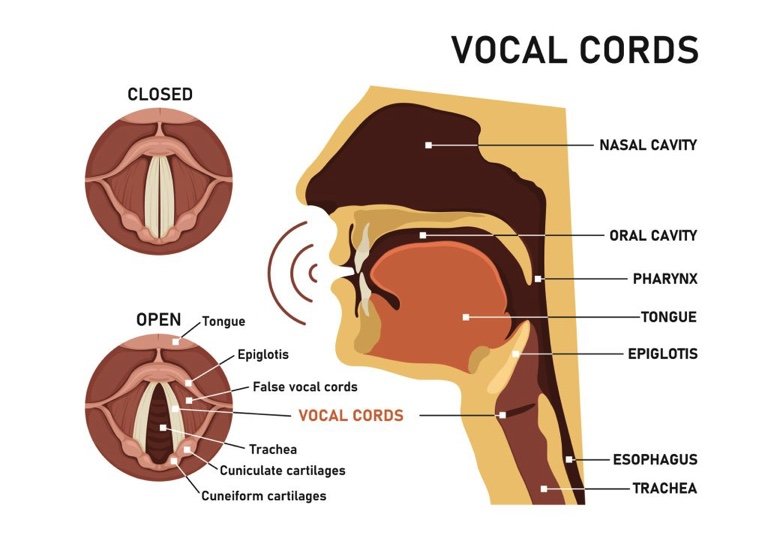
So what does that mean exactly? Well, your vocal cords are folds of muscular tissue located in your larynx, sitting right over your airway. Normally your vocal cords should come together when you speak, cough, or swallow. Otherwise, they should remain wide open to allow optimal breathing. With vocal cord dysfunction, your vocal cords are squeezing together during moments when they should be wide open. This narrows your throat, making it harder to breathe.
This squeezing or “contraction” of the vocal cords is usually brought on by some sort of trigger. Common triggers include:
exercise
environmental irritants such as smoke or exhaust
strong odors
very hot or cold temperatures
talking, coughing, or laughing
stress or anxiety
VCD symptoms usually come on quickly and dissipate quickly once the trigger is removed. Someone suffering a VCD “attack” may experience shortness of breath, hoarse voice, high-pitched breathing sounds, coughing, throat/chest tightness, and trouble getting air in.
Vocal cord dysfunction can take a huge toll on the quality of life, preventing sufferers from engaging in activities they once enjoyed. People often tell me that they have been avoiding exercise, social gatherings, or even going out in public altogether because they are afraid of having a VCD episode.
The good news is that it is possible for individuals with vocal cord dysfunction to gain control of their symptoms and live a normal life again. By learning more about their condition, finding ways to cope with its effects, and seeking out support when needed, people with VCD can take steps toward overcoming the difficulties associated with this disorder.
2. Causes Of Vocal Cord Dysfunction
So why do some people get Vocal Cord Dysfunction? What is causing this abnormal contraction of the vocal cords? The truth is, we don’t really know. Something causes the nerve and muscles of the larynx to become hypersensitive, with an easily triggered “close” reflex.
It’s common for people with VCD to also have a history of asthma, gastrointestinal reflux disease (GERD), post nasal drip (PND), upper respiratory infections, exposure to airborne chemicals, excess laryngeal muscle tension, and/or psychological factors such as high-stress levels or history of anxiety or trauma. We think experiencing one or some combination of these factors can bring about VCD. It’s possible that there may be different variants of VCD, each with different causes.
It’s also important to note that there may be a genetic component to VCD. Studies have shown that people with family members who suffer from VCD are more likely to develop the condition themselves. Genetics aside, lifestyle choices such as smoking or alcohol abuse can also increase the risk of developing VCD. Individuals who suffer from conditions like acid reflux disease (GERD) and chronic obstructive pulmonary disease (COPD) may also be at a higher risk for developing VCD.
By understanding the potential causes of VCD, individuals can work with their healthcare providers to identify potential triggers and develop effective treatment plans. With proper diagnosis and treatment, it is possible for those suffering from VCD to live symptom-free lives.
3. Symptoms Of Vocal Cord Dysfunction
Vocal cord dysfunction (VCD) can cause a range of symptoms that can significantly affect the quality of life. It’s important to be aware of the potential signs and symptoms in order to recognize VCD and begin treatment. In this section, we’ll explore what to look out for if you suspect you or someone you know may have VCD.
Common symptoms of VCD include severe shortness of breath, difficulty breathing while exercising, throat or chest tightness, wheezing or noisy breathing, coughing throat clearing, and intermittent voice hoarseness. People with VCD may find it especially hard to control their breathing during physical activity or when under stress. They might feel like they need to take very deep breaths or gasp for air at times.
It’s not just physical symptoms that can point toward VCD; there are often psychological aspects too. Feelings of anxiety related to breathing problems can become intense, especially if the person is unaware of what is causing their distress. These emotions may even lead to panic attacks or other mental health issues if left untreated. To make matters worse, the fear associated with having difficulty breathing can itself trigger further episodes of VCD!
The good news is that, although VCD can be scary in the moment, it is not something that is life-threatening. Although it really feels like you aren’t getting enough air, studies show that most of the time your blood oxygen levels are normal during a VCD attack. In very rare cases, I’ve heard of people losing consciousness during an attack. But as soon as the body becomes unconscious, the vocal cords pop wide open and you start breathing normally again.
If you think you might be experiencing signs or symptoms of VCD, it’s important to reach out to your doctor for help. They can diagnose the condition properly and point you in the right direction for treatment. With the right support and treatment plan in place, people struggling with vocal cord dysfunction can gain better control over their breathing.
4. Diagnosis Of Vocal Cord Dysfunction
Diagnosing vocal cord dysfunction (VCD) can be a challenging task. The only way to truly identify VCD is to observe the vocal cords through laryngoscopy (examining the vocal cords with a camera) during an episode. Can you imagine what the chances are of having a VCD episode while you are at your doctor’s office AND during the few minutes that they have a camera pointing down your throat? Nil. Therefore, VCD is usually diagnosed by ruling out every other potential cause.
The first step in diagnosing VCD is to take a detailed patient history. Patients should provide information about any lifestyle changes that may have contributed to their symptoms, such as exposure to irritants or emotional stress. Doctors also need to know if the patient has been diagnosed with any other medical conditions that could be causing the symptoms of VCD.
The next step is for the doctor to perform a physical exam and order tests to rule out other possible causes of the symptoms. Tests may include breathing tests, chest x-rays, and laryngoscopy. If all other potential causes are ruled out and the patient’s symptoms persist, then VCD may be diagnosed.
At the time of diagnosis of vocal cord dysfunction, individuals often feel confused and helpless. But there is hope: treatment options exist that can help manage or even resolve the condition. Read on for more information on the various treatment strategies and interventions available to those with vocal cord dysfunction.
5. Treatment Options For Vocal Cord Dysfunction
Okay, you’ve been diagnosed with vocal cord dysfunction. So how do we fix it? Well, in short, we need to create a relaxed larynx!! Certainly easier said than done, but it is possible. You have more control over your larynx than you think.
Based on your specific symptoms and triggers, your treatment plan may consist of one or more of the following options. Coordinate with your doctor and licensed speech-language pathologist to create a personalized plan that’s right for you.
Eliminate any external factors that can be irritating your vocal cords. Work with your doctor to properly treat your asthma, GERD, PND, or laryngeal infections. Avoid breathing in smoke or other harsh chemicals.
Stop traumatizing your vocal cords with coughing and throat clearing. Every time you cough or throat clear, you are slamming your vocal cords together. When you are coughing or your throat clearing excessively, all that slamming creates irritation. Reach out to a trained Speech Language Pathologist for cough and throat-clearing suppression techniques.
Release your stress in a healthy way. People often carry stress and tension in the neck and shoulders. This can lead to tense muscles at and around the vocal cords too. Look for healthy ways to release tension build-up. Daily exercise, meditation, and talking to someone about your stressors (ideally a trained psychologist or cognitive behavioral therapist) can help. It’s also important to seek out support from family and friends who understand your struggles and can provide emotional support.
Get breathing retraining. People with VCD often have a generally disordered breathing pattern. It’s a bit of a chicken or the egg situation; does disordered breathing cause VCD or does VCD cause symptoms of disordered breathing? We don’t know. But what we do know is that teaching people healthier ways to breathe can decrease and even eliminate symptoms of VCD.
If your VCD is exercise-induced, we tend to classify it as EILO (exercise-induced laryngeal obstruction). Learning to incorporate healthy breathing patterns into your exercise regime or into your sport is essential to controlling the VCD. Look for a Speech Language Pathologist with specialty training in VCD and breathing.
Use a healthy speaking voice. People with VCD are prone to using excess muscle tension when speaking. This primes the vocal cords for that abnormal “squeeze” reflex. Work with a Speech Language Pathologist to learn to use your vocal cords in a relaxed way when speaking.
Vocal cord dysfunction is a disorder that you can overcome with proper care and attention given by a professional healthcare provider. Once VCD is diagnosed, reaching out to a specialty trained Speech Language Pathologist (SLP) is highly recommended. Your SLP will build a treatment program individualized to you and your specific triggers and needs. Successful VCD therapy programs should be a multi-pronged approach addressing the physical, emotional, and intellectual components of the disorder.
Conclusion
To wrap it up, vocal cord dysfunction can have long-term implications that negatively impact the quality of life. If you believe you or a loved one may have VCD, follow up with a doctor to get it properly diagnosed, and start taking steps toward improving symptoms now.
The good news is that therapies are available to treat the condition and help you breathe normally again. In my practice I have seen young athletes reunited with the sport that they love, retirees regain the confidence to live active and fulfilling lives, teachers return to the classroom after eliminating their chronic cough, and so many more wonderful outcomes. With proper diagnosis, treatment, and management, you too have the power to overcome VCD.