Is Sleep-Disordered Breathing The Same As Sleep Apnea?
Sleep-related breathing disorders are a common group of conditions that affect many individuals worldwide. Among them, sleep disordered breathing (SDB) and sleep apnea are two terms that are often used interchangeably, but they have distinct differences. As a speech language pathologist, I’ve found that many of my patients also struggle with some sort of sleep-disordered breathing. So in this blog post, we will explore the different types of sleep disordered breathing to help shed some light on these all-to-common conditions.
What Is Sleep-Disordered Breathing?
Sleep disordered breathing (SDB) is a general term that encompasses a wide range of breathing abnormalities during sleep. It can refer to any disruption in the normal breathing pattern during sleep, including partial or complete blockage of the airway, irregular breathing, or abnormal breathing effort. Here are some of the common types of sleep-disordered breathing:
Obstructive Sleep Apnea (OSA): This is the most common type of sleep-disordered breathing. OSA occurs when there is a partial or complete blockage of the upper airway during sleep, resulting in pauses in breathing, often accompanied by loud snoring, gasping, or choking. These pauses in breathing can lead to reduced oxygen levels in the blood and disrupt the normal sleep pattern, leading to daytime sleepiness, fatigue, and other health issues.
Central Sleep Apnea (CSA): Unlike OSA, CSA is not related to an obstruction in the airway. Instead, it occurs when the brain fails to send proper signals to the muscles that control breathing during sleep. This results in pauses in breathing without any effort to breathe, and it is less common than OSA. CSA is often associated with certain medical conditions, such as heart failure, brainstem lesions, or central nervous system disorders.
Complex Sleep Apnea Syndrome (CSAS): Also known as treatment-emergent central sleep apnea, CSAS is a combination of OSA and CSA. It initially presents as OSA but may transition to CSA after continuous positive airway pressure (CPAP) therapy is initiated. The underlying cause of this transition is not fully understood and may require further evaluation and treatment adjustments.
Upper Airway Resistance Syndrome (UARS): UARS is characterized by partial blockage of the upper airway during sleep, leading to increased effort to breathe and disrupted sleep. It may not meet the criteria for a diagnosis of sleep apnea, but it can still cause symptoms such as snoring, fragmented sleep, and daytime sleepiness.
Snoring: Although snoring is not always considered a sleep-disordered breathing condition, it can sometimes be a sign of an underlying issue. Snoring occurs when there is partial blockage of the airway during sleep, leading to vibrations of the throat tissues that produce the sound of snoring. In some cases, snoring can progress to more severe forms of SDB, such as OSA.
Signs and symptoms of SDB may include snoring, gasping or choking during sleep, restless tossing and turning, frequent awakenings during the night, daytime sleepiness, morning headaches, and irritability. However, it's important to note that SDB can sometimes be asymptomatic or have mild symptoms, making it challenging to detect without proper evaluation and diagnosis.
What is Sleep Apnea
Sleep apnea is a specific type of sleep disordered breathing that is characterized by repetitive episodes of partial or complete blockage of the airway during sleep, leading to interrupted breathing (apneas) and disrupted sleep. Sleep apnea is often associated with loud snoring, abrupt awakenings accompanied by choking or gasping, restless sleep, excessive daytime sleepiness, morning headaches, difficulty concentrating, and irritability. In stark contrast to normal snoring patterns, loud gasps for air or pauses in breathing at night may be present. These episodes can sometimes last as long as 10 seconds or more and occur several times throughout the night. It is a serious condition that can have significant health consequences if left untreated, including increased risk of cardiovascular disease, diabetes, mood disorders, and impaired cognitive function.
Causes Of Sleep Disordered Breathing
Causes of sleep-disordered breathing can vary and be multifactorial. Common causes include:
Obesity: Excess body weight, particularly in the neck and upper airway, can increase the risk of sleep-disordered breathing, including obstructive sleep apnea (OSA) and upper airway resistance syndrome (UARS) (Young et al., 2002).
Anatomical abnormalities: Structural abnormalities in the upper airway, such as enlarged tonsils, adenoids, deviated septum, or narrow airway, can contribute to sleep-disordered breathing by causing partial or complete blockage of the airway during sleep (Jordan et al., 2005).
Age and gender: Sleep-disordered breathing tends to be more prevalent in older adults and males, although it can occur in individuals of any age and gender (Redline et al., 1997; Peppard et al., 2000).
Genetic factors: There is evidence to suggest that certain genetic factors may predispose individuals to sleep-disordered breathing. Family history of sleep apnea and genetic variants related to upper airway anatomy and respiratory control have been identified as potential risk factors (Patel et al., 2018).
Alcohol and sedatives: Consuming alcohol or sedatives before bedtime can relax the muscles in the upper airway, leading to increased collapsibility of the airway and increased risk of sleep-disordered breathing (Bhattacharyya et al., 2014).
Medical conditions: Certain medical conditions, such as obesity hypoventilation syndrome, congestive heart failure, hypothyroidism, acromegaly, and neuromuscular disorders, can contribute to sleep-disordered breathing (Mokhlesi et al., 2017).
Lifestyle factors: Poor sleep hygiene, irregular sleep patterns, and sleep deprivation can also disrupt the normal breathing pattern during sleep and contribute to sleep-disordered breathing (Young et al., 2003).
Diagnosis of Sleep Disordered Breathing
Sleep disordered breathing, if left untreated, can have serious health consequences. The repeated interruptions in breathing during sleep can lead to decreased oxygen levels in the blood, which can strain the heart and other organs. Over time, this can increase the risk of developing high blood pressure, cardiovascular disease, stroke, and type 2 diabetes. SDB has also been linked to mood disorders such as depression and anxiety, cognitive impairments, decreased quality of life, and an increased risk of accidents due to daytime sleepiness.
If you suspect you may have sleep disordered breathing, it's important to seek a proper diagnosis from a healthcare professional. Diagnosis typically involves a sleep study, which can be done at a sleep center or in some cases, at home using a portable monitoring device. The sleep study monitors various parameters during sleep, such as brain activity, eye movement, heart rate, oxygen levels, and airflow, to determine the presence and severity of SDB.
Treatments For Sleep Disordered Breathing
Treatment options for sleep disordered breathing depend on the severity of the condition and may include lifestyle changes, positional therapy, oral appliances, continuous positive airway pressure (CPAP) therapy, and in some cases, surgery. Lifestyle changes may include losing weight, avoiding alcohol and sedatives before bedtime, sleeping in a different position, and practicing good sleep hygiene.
As I said earlier, I encounter many patients in my practice that are also suffering from SDB; likely because most of my patients are coming to me for some sort of underlying neurological condition or orophayrngeal dysfunction. In conjunction with the above listed treatments, breathing retraining therapy can also be a powerful tool for controlling SDB.
Breathing Retraining Therapy
Specialty trained speech language pathologists, such as Eloquium Speech Therapy, may provide breathing retraining exercises to individuals with SDB. This may involve teaching proper breathing techniques, such as diaphragmatic breathing, nasal breathing, and slow, controlled breathing, to help individuals establish healthy breathing patterns during both wakefulness and sleep. Breathing retraining can help improve the coordination and efficiency of respiratory muscles, reduce respiratory effort, and enhance overall lung function, which can have a positive impact on sleep quality. (Guillen et al., 2015; Camacho et al., 2021).
If you suspect you may have sleep disordered breathing, consulting with a qualified speech therapist as part of a comprehensive treatment team can be beneficial in addressing the overall symptoms of the condition.
Prevention is Better
While sleep disordered breathing is a common condition, there are steps you can take to reduce your risk of developing it. Maintaining a healthy lifestyle, including regular exercise, maintaining a healthy weight, avoiding smoking and excessive alcohol consumption, and practicing good sleep hygiene, such as establishing a consistent sleep schedule and creating a conducive sleep environment, can all help promote healthy sleep patterns and reduce the risk of sleep disordered breathing.
Conclusion
So to wrap up, sleep disordered breathing is a common condition that affects many people, yet often goes unnoticed or untreated. It can have serious health consequences if left untreated, including cardiovascular disease, mood disorders, and cognitive impairments. If you suspect you may have sleep disordered breathing, it's important to seek a proper diagnosis from a healthcare professional and discuss appropriate treatment options. Remember, prioritizing good sleep hygiene and adopting a healthy lifestyle can go a long way in preventing sleep disordered breathing and promoting overall health and well-being. So, take a step towards breathing easy and getting a restful night's sleep!
Chronic Cough. Is It Neurogenic?
What is Chronic Cough?
Chronic Cough simply means a cough that lasts longer than 8 weeks. There are many reasons why people can end up with a chronic cough. Well known causes of chronic cough include COPD, viral infection, post nasal drip, asthma, GERD, and more. But did you know that chronic cough can also be neurogenic in origin? Neurogenic cough (also known as Laryngeal Hyperresponsiveness or Neurogenic Laryngeal Hypersensitivity) is a condition in which the nerve that innervates the larynx becomes hypersensitive, causing you to cough more frequently.
What is Neurogenic Cough?
The vagus nerve is the longest cranial nerve in your body and it has many different functions. It sends taste signals to the brain, sends motor signals to the soft palate and larynx, and even helps to regulate digestion and heart rhythm. It also sends sensory information from your throat (your larynx) to your brain. This is an important job! When there is something in your throat that shouldn’t be there, like mucus or food, the vagus nerve senses it and sends a signal to the brain saying, “Help! There’s a foreign body in our throat! We need to cough!!” Then, fast as lightning, the brain responds by sending a cough reflex down to the larynx. Cough! This is what is happening when we swallow something down wrong or when we get a cold and have mucus to cough up. But with Neurogenic cough, the vagus nerve has become so hypersensitive that even the smallest stimulus (cold air, a strong scent, normal body secretions, or vibrations from talking) can now trigger a cough. This often means that people with neurogenic cough end up coughing all the time! In fact, the cough can be so severe that it can truly disrupt quality of life.
So what causes the vagus nerve to become so hypersensitized?
Great question. There is a lot of new research going on right now about what causes Neurogenic cough and how to fix it. It is believed that inflammatory, infective, or allergic factors (or some combination) can create a hypersensitive nerve. Initial causes may include an upper respiratory tract infection, inhalation of toxic fumes, allergic reactions, and more. But once the vagus nerve has become hypersensitized, the cough itself can then make it worse! The constant coughing can cause increased laryngeal inflammation, making the nerve even more sensitive, which leads to more coughing. I call it the “runaway cough train” and it can lead to a chronic severe cough that lasts months or even years.
What can people suffering from Neurogenic cough do about it?
First it’s important to get an accurate diagnosis. Your doctor needs to rule out any other possible factors that could be causing your cough. They will work with you to eliminate anything causing inflammation or irritation to your throat. This might include prescribing medications to reduce post nasal drip, GERD, or seasonal allergies. If you end up with a diagnosis of Neurogenic cough, your doctor will likely refer you to a specialty trained Speech Pathologist for behavioral cough therapy, including breathing retraining and cough suppression training. These therapies consist of strategies to help you stifle the cough, so that you can start to slow that runaway cough train and allow the vagus nerve time to heal. Aside from behavioral cough therapy, your doctor may prescribe a neuromodulator medication to reduce the nerve sensitivity or they may even suggest performing a superior laryngeal nerve block to dull the reactiveness of one section of your vagus nerve.
Conclusion
If you or a loved one is diagnosed with Neurogenic chronic cough, fear not. Gaining control of your cough is possible! Reach out to a specialty trained Speech Language Pathologist to help you stop the runaway cough train and put you on the track to wellness.
When Should I Seek Help For a Vocal Disorder?
What is causing my chronic cough?
If you’ve been feeling like your voice isn’t what it used to be – uneven pitch, reduced range in speaking or singing, hoarseness – don’t delay in seeking help. Dysphonia (impairment of voice production) can have a variety of different causes such as inflammation, abnormalities of the vocal tract, neurological conditions, or excess muscle tension. Addressing the problem right away gives you the best odds for successful treatment, ensuring any issues won’t become more serious over time.
When to Seek Help
If you are struggling with dysphonia that persists for more than two weeks, it is important to seek professional medical assistance from an Otolaryngologist (ENT specialist). ENTs are physicians that specialize in the care of the ears, nose, and throat. While it can be alarming to go to the doctor for a voice issue, seeking the expertise of an ENT physician can help you discover why your voice isn’t performing as normal and bring you relief. Knowledge is power! Your ENT can diagnose the problem and point you in the right direction for help.
Some signs and symptoms to look out for include:
• Persistent changes in vocal quality, or difficulty speaking
• Loss of vocal range, volume, or pitch control
• Painful or uncomfortable sensations when speaking or singing
• A foreign body sensation in the throat while speaking
• Chronic coughing or throat clearing during speech/singing
• Fatigue from voice use (after extended periods of talking)
Depending on the diagnosis, the next step may be referral to a Speech-Language Pathologist (SLP) for Voice Therapy. Your SLP typically conducts a voice evaluation to determine what is causing the disorder and how best to treat it. Eloquium Speech Therapy can help with this.
Treatment plans are individualized and designed specifically to meet your particular needs – they may involve exercises that improve vocal quality and instruction on how to conserve and modify your speaking behavior. More often than not, these strategies can be incredibly helpful in improving voice issues and can make all the difference in restoring a strong, functional voice.
Conclusion
If you are experiencing any signs or symptoms of a voice disorder, it is important to seek professional help right away. An Otolaryngologist can provide an accurate diagnosis and referral to the appropriate specialist in order to begin treatment. If your doctor feels that Voice Therapy may help, reach out to a voice trained Speech Language Pathologist. Voice Therapy can improve vocal quality, strength, and endurance.
Understanding and Overcoming Vocal Cord Dysfunction
What is causing my chronic cough?
Most patients who come to my practice with Vocal Cord Dysfunction have never heard of it prior to their diagnosis. What is VCD? How did I get it? What are my treatment options? VCD is a disorder of the upper airway where the vocal cords fail to function properly, leading to difficulty breathing.
It is a surprisingly common condition that can cause immense physical and emotional distress to those who have it. Unfortunately, VCD can be difficult to diagnose, leaving many people feeling frustrated and confused about what is going on within their bodies. By understanding more about this condition and taking steps to seek help, you can find relief.
In this article, we’ll explore what vocal cord dysfunction is, the impact it can have on someone’s life, and ways to manage the symptoms. We’ll also look at how to identify the signs of VCD in you or someone you love and how to get the support you need to gain control of your breathing. Keep reading for everything you need to know about vocal cord dysfunction!
1. What Is Vocal Cord Dysfunction?
Vocal Cord Dysfunction (VCD) is an umbrella term for dysfunctional movement of the vocal cords. It goes by many names such as Paradoxical Vocal Fold Motion (PVFM), Exercise Induced Laryngeal Obstruction (EILO), Episodic Laryngospasm, Inducible Laryngeal Obstruction (ILO), and more. All of these terms are used to describe an intermittent, abnormal narrowing of the larynx.
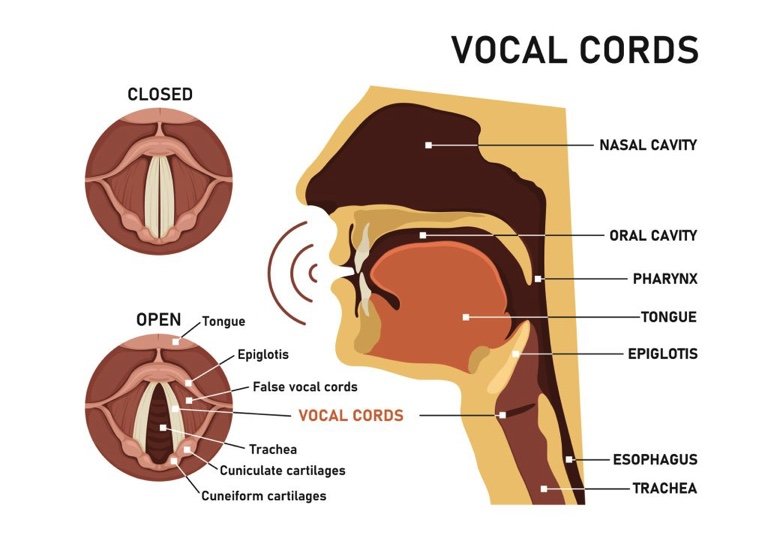
So what does that mean exactly? Well, your vocal cords are folds of muscular tissue located in your larynx, sitting right over your airway. Normally your vocal cords should come together when you speak, cough, or swallow. Otherwise, they should remain wide open to allow optimal breathing. With vocal cord dysfunction, your vocal cords are squeezing together during moments when they should be wide open. This narrows your throat, making it harder to breathe.
This squeezing or “contraction” of the vocal cords is usually brought on by some sort of trigger. Common triggers include:
exercise
environmental irritants such as smoke or exhaust
strong odors
very hot or cold temperatures
talking, coughing, or laughing
stress or anxiety
VCD symptoms usually come on quickly and dissipate quickly once the trigger is removed. Someone suffering a VCD “attack” may experience shortness of breath, hoarse voice, high-pitched breathing sounds, coughing, throat/chest tightness, and trouble getting air in.
Vocal cord dysfunction can take a huge toll on the quality of life, preventing sufferers from engaging in activities they once enjoyed. People often tell me that they have been avoiding exercise, social gatherings, or even going out in public altogether because they are afraid of having a VCD episode.
The good news is that it is possible for individuals with vocal cord dysfunction to gain control of their symptoms and live a normal life again. By learning more about their condition, finding ways to cope with its effects, and seeking out support when needed, people with VCD can take steps toward overcoming the difficulties associated with this disorder.
2. Causes Of Vocal Cord Dysfunction
So why do some people get Vocal Cord Dysfunction? What is causing this abnormal contraction of the vocal cords? The truth is, we don’t really know. Something causes the nerve and muscles of the larynx to become hypersensitive, with an easily triggered “close” reflex.
It’s common for people with VCD to also have a history of asthma, gastrointestinal reflux disease (GERD), post nasal drip (PND), upper respiratory infections, exposure to airborne chemicals, excess laryngeal muscle tension, and/or psychological factors such as high-stress levels or history of anxiety or trauma. We think experiencing one or some combination of these factors can bring about VCD. It’s possible that there may be different variants of VCD, each with different causes.
It’s also important to note that there may be a genetic component to VCD. Studies have shown that people with family members who suffer from VCD are more likely to develop the condition themselves. Genetics aside, lifestyle choices such as smoking or alcohol abuse can also increase the risk of developing VCD. Individuals who suffer from conditions like acid reflux disease (GERD) and chronic obstructive pulmonary disease (COPD) may also be at a higher risk for developing VCD.
By understanding the potential causes of VCD, individuals can work with their healthcare providers to identify potential triggers and develop effective treatment plans. With proper diagnosis and treatment, it is possible for those suffering from VCD to live symptom-free lives.
3. Symptoms Of Vocal Cord Dysfunction
Vocal cord dysfunction (VCD) can cause a range of symptoms that can significantly affect the quality of life. It’s important to be aware of the potential signs and symptoms in order to recognize VCD and begin treatment. In this section, we’ll explore what to look out for if you suspect you or someone you know may have VCD.
Common symptoms of VCD include severe shortness of breath, difficulty breathing while exercising, throat or chest tightness, wheezing or noisy breathing, coughing throat clearing, and intermittent voice hoarseness. People with VCD may find it especially hard to control their breathing during physical activity or when under stress. They might feel like they need to take very deep breaths or gasp for air at times.
It’s not just physical symptoms that can point toward VCD; there are often psychological aspects too. Feelings of anxiety related to breathing problems can become intense, especially if the person is unaware of what is causing their distress. These emotions may even lead to panic attacks or other mental health issues if left untreated. To make matters worse, the fear associated with having difficulty breathing can itself trigger further episodes of VCD!
The good news is that, although VCD can be scary in the moment, it is not something that is life-threatening. Although it really feels like you aren’t getting enough air, studies show that most of the time your blood oxygen levels are normal during a VCD attack. In very rare cases, I’ve heard of people losing consciousness during an attack. But as soon as the body becomes unconscious, the vocal cords pop wide open and you start breathing normally again.
If you think you might be experiencing signs or symptoms of VCD, it’s important to reach out to your doctor for help. They can diagnose the condition properly and point you in the right direction for treatment. With the right support and treatment plan in place, people struggling with vocal cord dysfunction can gain better control over their breathing.
4. Diagnosis Of Vocal Cord Dysfunction
Diagnosing vocal cord dysfunction (VCD) can be a challenging task. The only way to truly identify VCD is to observe the vocal cords through laryngoscopy (examining the vocal cords with a camera) during an episode. Can you imagine what the chances are of having a VCD episode while you are at your doctor’s office AND during the few minutes that they have a camera pointing down your throat? Nil. Therefore, VCD is usually diagnosed by ruling out every other potential cause.
The first step in diagnosing VCD is to take a detailed patient history. Patients should provide information about any lifestyle changes that may have contributed to their symptoms, such as exposure to irritants or emotional stress. Doctors also need to know if the patient has been diagnosed with any other medical conditions that could be causing the symptoms of VCD.
The next step is for the doctor to perform a physical exam and order tests to rule out other possible causes of the symptoms. Tests may include breathing tests, chest x-rays, and laryngoscopy. If all other potential causes are ruled out and the patient’s symptoms persist, then VCD may be diagnosed.
At the time of diagnosis of vocal cord dysfunction, individuals often feel confused and helpless. But there is hope: treatment options exist that can help manage or even resolve the condition. Read on for more information on the various treatment strategies and interventions available to those with vocal cord dysfunction.
5. Treatment Options For Vocal Cord Dysfunction
Okay, you’ve been diagnosed with vocal cord dysfunction. So how do we fix it? Well, in short, we need to create a relaxed larynx!! Certainly easier said than done, but it is possible. You have more control over your larynx than you think.
Based on your specific symptoms and triggers, your treatment plan may consist of one or more of the following options. Coordinate with your doctor and licensed speech-language pathologist to create a personalized plan that’s right for you.
Eliminate any external factors that can be irritating your vocal cords. Work with your doctor to properly treat your asthma, GERD, PND, or laryngeal infections. Avoid breathing in smoke or other harsh chemicals.
Stop traumatizing your vocal cords with coughing and throat clearing. Every time you cough or throat clear, you are slamming your vocal cords together. When you are coughing or your throat clearing excessively, all that slamming creates irritation. Reach out to a trained Speech Language Pathologist for cough and throat-clearing suppression techniques.
Release your stress in a healthy way. People often carry stress and tension in the neck and shoulders. This can lead to tense muscles at and around the vocal cords too. Look for healthy ways to release tension build-up. Daily exercise, meditation, and talking to someone about your stressors (ideally a trained psychologist or cognitive behavioral therapist) can help. It’s also important to seek out support from family and friends who understand your struggles and can provide emotional support.
Get breathing retraining. People with VCD often have a generally disordered breathing pattern. It’s a bit of a chicken or the egg situation; does disordered breathing cause VCD or does VCD cause symptoms of disordered breathing? We don’t know. But what we do know is that teaching people healthier ways to breathe can decrease and even eliminate symptoms of VCD.
If your VCD is exercise-induced, we tend to classify it as EILO (exercise-induced laryngeal obstruction). Learning to incorporate healthy breathing patterns into your exercise regime or into your sport is essential to controlling the VCD. Look for a Speech Language Pathologist with specialty training in VCD and breathing.
Use a healthy speaking voice. People with VCD are prone to using excess muscle tension when speaking. This primes the vocal cords for that abnormal “squeeze” reflex. Work with a Speech Language Pathologist to learn to use your vocal cords in a relaxed way when speaking.
Vocal cord dysfunction is a disorder that you can overcome with proper care and attention given by a professional healthcare provider. Once VCD is diagnosed, reaching out to a specialty trained Speech Language Pathologist (SLP) is highly recommended. Your SLP will build a treatment program individualized to you and your specific triggers and needs. Successful VCD therapy programs should be a multi-pronged approach addressing the physical, emotional, and intellectual components of the disorder.
Conclusion
To wrap it up, vocal cord dysfunction can have long-term implications that negatively impact the quality of life. If you believe you or a loved one may have VCD, follow up with a doctor to get it properly diagnosed, and start taking steps toward improving symptoms now.
The good news is that therapies are available to treat the condition and help you breathe normally again. In my practice I have seen young athletes reunited with the sport that they love, retirees regain the confidence to live active and fulfilling lives, teachers return to the classroom after eliminating their chronic cough, and so many more wonderful outcomes. With proper diagnosis, treatment, and management, you too have the power to overcome VCD.